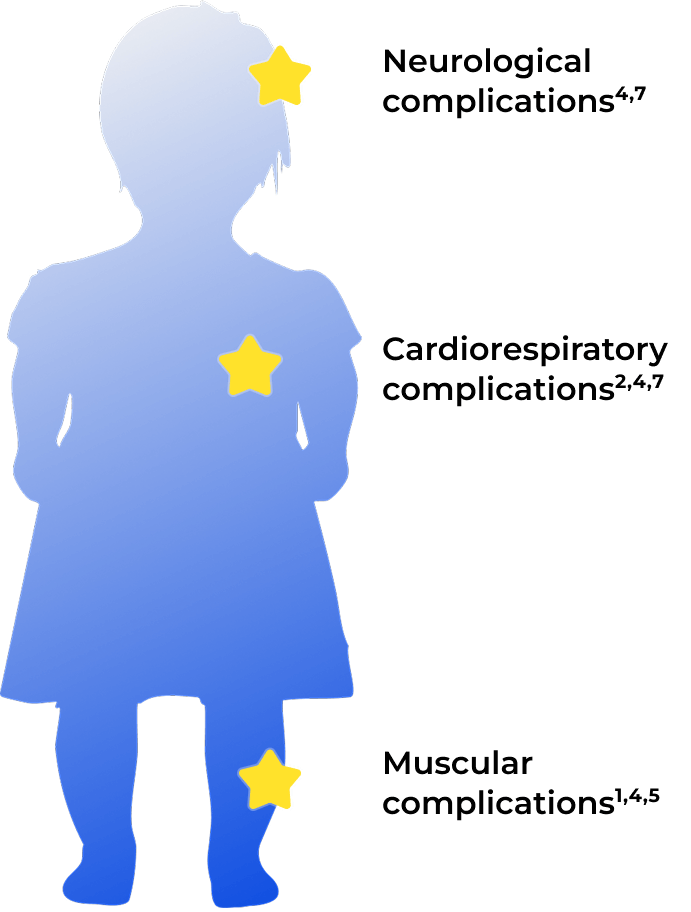
Achondroplasia in children demands monitoring of multiple complex health complications.1
Caused by a systemic FGFR3 variant, the impact of achondroplasia extends beyond skeletal dysplasia. Taking a multidisciplinary approach supports better outcomes and quality of life for those living with it.1-4
Achondroplasia is about bones and beyond. Discover the full impact of living with achondroplasia.3,4
Genetics of achondroplasia
Achondroplasia is a rare genetic condition arising from a systemic FGFR3 variant. It can cause serious muscular, neurological, and cardiorespiratory complications in addition to the well-characterized skeletal dysplasia.1,4-9
Explore how the constitutive activation of FGFR3 throughout the body can have a broader impact beyond skeletal dysplasia.
Explore how the constitutive activation of FGFR3 throughout the body can have a broader impact beyond skeletal dysplasia.
Learn more about FGFR3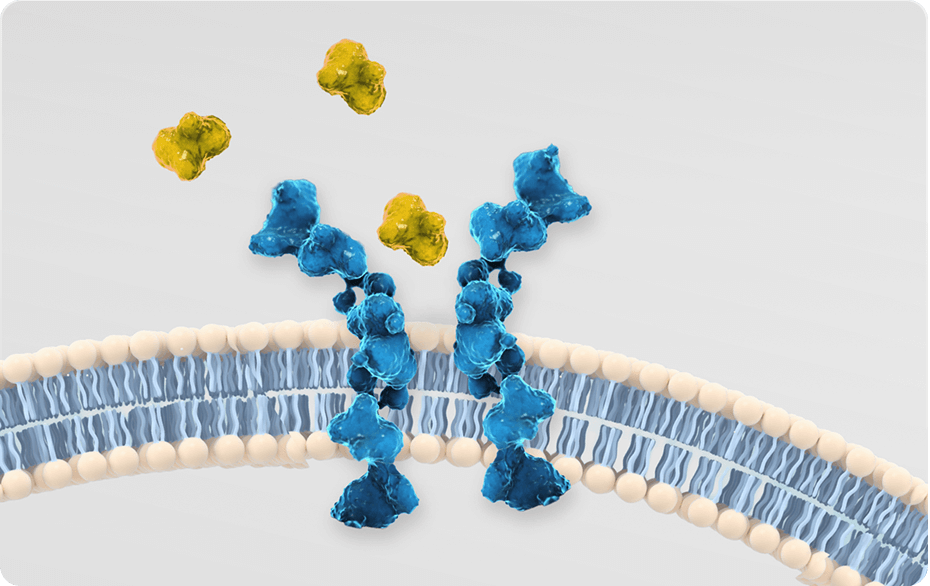
Impact of achondroplasia
Achondroplasia can present with a range of clinical manifestations and lead to lifelong health complications. These complications may profoundly diminish function and quality of life.4,9-11
Delve into the many health and psychosocial consequences of achondroplasia.
Managing achondroplasia
The achondroplasia treatment landscape is rapidly evolving. Today’s management aims to address different characteristics of the condition, ranging from clinical manifestations to aspects of health-related quality of life.12
Explore the importance of addressing FGFR3 in achondroplasia.


Helpful resources
Find resources to expand your understanding of achondroplasia, and tools to help support your patients and their families.
FGFR3=fibroblast growth factor receptor 3.
References:
1. Savarirayan R, Ireland P, Irving M, et al. International Consensus Statement on the diagnosis, multidisciplinary management and lifelong care of individuals with achondroplasia. Nat Rev Endocrinol. 2022;18:173-189.
2. Pauli RM. Achondroplasia: a comprehensive clinical review. Orphanet J Rare Dis. 2019;14(1):1-49.
3. McDonald EJ, De Jesus O. Achondroplasia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 23, 2023. Accessed July 2025. https://www.ncbi.nlm.nih.gov/books/NBK559263
4. Ireland PJ, Pacey V, Zankl A, et al. Optimal management of complications associated with achondroplasia. Appl Clin Genet. 2014;7:117-125.
5. Horton WA, Hall JG, Hecht JT. Achondroplasia. Lancet. 2007;370(9582):162-172.
6. Sims DT, Onambélé-Pearson GL, Burden A, et al. Specific force of the vastus lateralis in adults with achondroplasia. J Appl Physiol. 2018;124(3):696-703.
7. Baujat G, Legeai-Mallet L, Finidori G, et al. Achondroplasia. Best Pract Res Clin Rheumatol. 2008;22(1):3-18.
8. Cormier-Daire V, AlSayed M, Alves I, et al. Optimising the diagnosis and referral of achondroplasia in Europe: European Achondroplasia Forum best practice recommendations. Orphanet J Rare Dis. 2022;17(1):293.
9. Murton MC, Drane ELA, Goff-Leggett DM, et al. Burden and treatment of achondroplasia: a systematic literature review. Adv Ther. 2023;40(9):3639-3680.
10. McGraw SA, Henne JC, Nutter J, et al. Treatment goals for achondroplasia: a qualitative study with parents and adults. Adv Ther. 2022;39(7):3378-3391.
11. Hoover-Fong J, Cheung MS, Fano V, et al. Lifetime impact of achondroplasia: current evidence and perspectives on the natural history. Bone. 2021;146:115872.
12. Wrobel W, Pach E, Ben-Skowronek I. Advantages and disadvantages of different treatment methods in achondroplasia: a review. Int J Mol Sci. 2021;22(11):5573.